Diabetic foot ulcers can be a significant concern for individuals with diabetes. These chronic wounds can cause pain and discomfort and even lead to the amputation of a limb. Therefore, individuals with diabetes must take extra care of their feet to prevent the development of foot ulcers.
Self-care plays an essential role in managing diabetic foot ulcers and can help to reduce the risk of complications. However, many individuals with diabetes may not be aware of self-care practices that can effectively prevent and treat diabetic foot ulcers.
This article will explore self-care tips for diabetic foot ulcers. It will provide practical advice on how to take care of your feet, including the importance of proper foot hygiene, using appropriate footwear, and managing blood sugar levels.
It will also provide evidence-based recommendations to help individuals with diabetes in effectively managing their foot health. By implementing these self-care practices, individuals can take control of their foot ulcer, promote healing, prevent complications, and improve their overall foot health.
Also read: Why Ignoring Diabetic Foot Ulcers is not Advisable?
Common causes of diabetic foot ulcers
Diabetic foot ulcers occur when people with diabetes have problems with the nerves or blood vessels in their feet, which can lead to toe ulcers. The common causes of diabetic foot ulcers are:
Nerve-related issues
Elevated glucose (hyperglycemia) levels in the blood can impact the sensory nerves negatively, which may lead to peripheral neuropathy.
Peripheral neuropathy is a disorder that impacts the nerves in extreme parts of our body, particularly in the hands and feet. This condition can cause changes in sensation or a complete loss of feeling, resulting in an inability to detect pain.
It is estimated that around half of all adults with diabetes will experience peripheral neuropathy, increasing the risk of foot injuries from pressure, cuts, or bruises resulting in foot ulcers.
Blood circulation issues
Long-term elevated blood sugar levels can harm blood vessels, causing a decline in blood supply to the feet and skin, leading to toe ulcers. The issue in blood circulation can delay wound healing.
Risk factors for diabetic foot ulcers
Individuals diagnosed with diabetes must remain cautious as they are susceptible to developing foot ulcers with various underlying causes. Several factors contribute to the increased likelihood of foot ulcers, such as:
- Peripheral artery disease (PAD): Reduced blood flow to the legs and feet, commonly seen in individuals with diabetes, can impair the healing process and increase the risk of ulcers.
- Foot deformities: Structural abnormalities like bunions, hammertoes, or Charcot’s foot can create pressure points or areas of friction that make the skin more susceptible to damage.
- Poor circulation: Impaired blood circulation, often associated with diabetes and PAD, hampers the delivery of nutrients and oxygen to the feet, hindering wound healing.
- Foot care neglect: Poor foot hygiene, inadequate nail care, wearing improper footwear, and lack of regular foot inspections contribute to the risk of developing ulcers.
- Previous history of ulcers or amputation: If you have had a foot ulcer or amputation in the past, the likelihood of future ulcers increases.
What are the stages of diabetic foot ulcers?
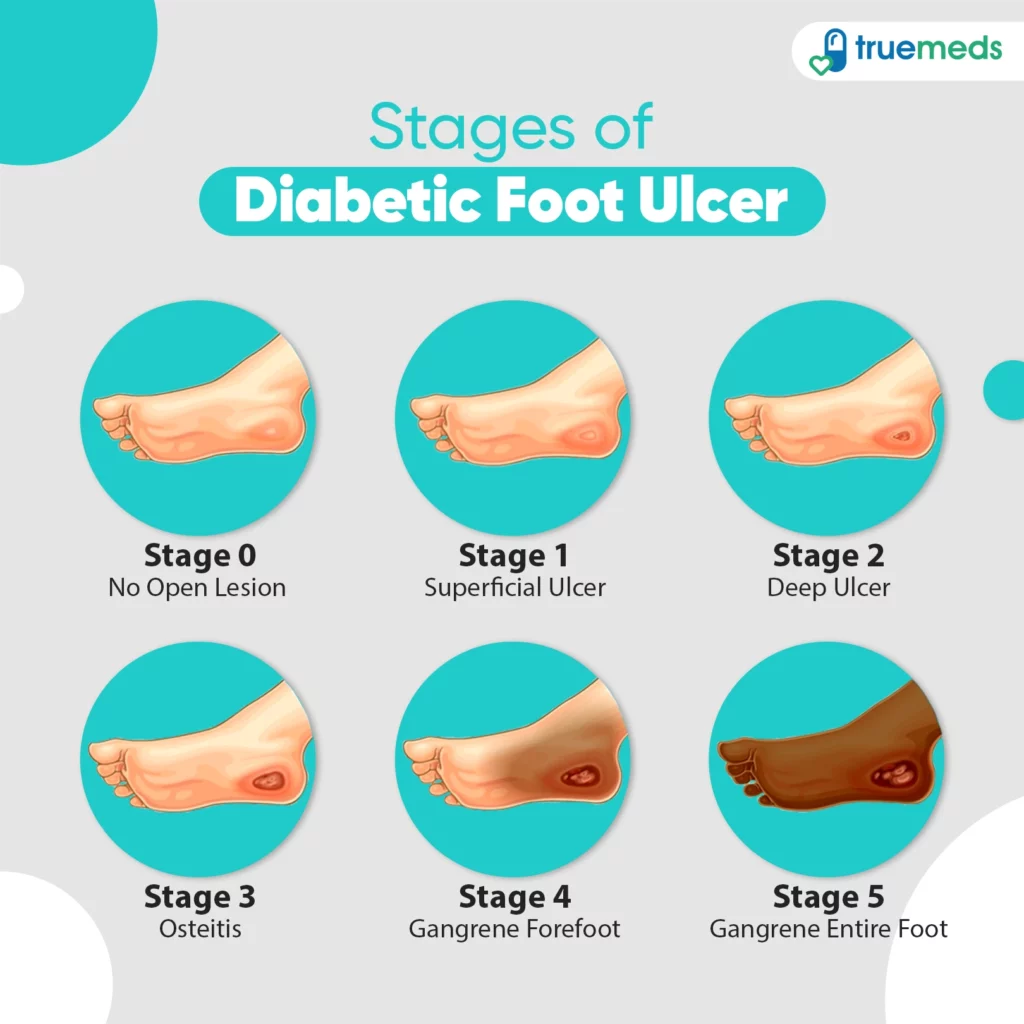
Diabetic foot ulcers can be classified into different stages based on their severity. The most commonly used classification includes the following stages:
- Stage 0: Skin may show signs of redness and swelling (redness that does not fade when pressure is applied).
- Stage 1: Ulcer is shallow, typically without the involvement of underlying structures.
- Stage 2: Ulcer extends deeper, involving ligaments, tendons, or joint capsules.
- Stage 3: Ulcer extends to deeper structures, such as bones or joints.
- Stage 4: Partial foot gangrene, typically affecting the toes or forefoot.
- Stage 5: Extensive gangrene (the affected tissue turns black and starts decaying) involving the entire foot.
Steps for self-diabetic foot ulcer treatment
Self-diabetic foot ulcer treatment involves several essential steps to promote healing and prevent complications. Here are the key steps to follow:
Step 1: Cleanse and inspect regularly
Gently wash the ulcer with mild soap and lukewarm water to keep the area clean. Refrain from scrubbing the area as it may cause further irritation. Ensure to examine the ulcer daily for any signs of infection.
Step 2: Protect and relieve pressure
To safeguard the ulcer from further harm, opting for suitable footwear, such as well-fitted shoes or therapeutic footwear that a healthcare expert has suggested, is advisable. This will help protect the area and keep it from getting worse.
Step 3: Dressing and wound care
It is essential to stick to the instructions provided by your healthcare provider when dressing and caring for your wounds. Regularly changing dressings using sterile techniques is crucial in preventing infection. Sometimes, your doctor may recommend using specialised dressings that can help promote moist healing.
Also read: Infected Wound Symptoms and Treatment
Step 4: Managing blood sugar levels
Maintaining blood sugar levels within the recommended range suggested by your healthcare provider is essential. Monitor your blood glucose levels regularly, adhere to the prescribed medication or insulin regimen, and follow a healthy and balanced diabetic diet.
Also read: Foods to Regulate Blood Sugar
Step 5: Promoting overall foot health
Maintaining proper foot hygiene ensures healthy feet. It is recommended to regularly clean and dry your feet and be mindful when trimming your nails. Additionally, it is essential to moisturise dry skin to prevent cracking. Protecting your feet from extreme temperatures and potential injuries is also important.
Promising treatments for diabetic foot ulcers
There are several promising treatments available for diabetic foot ulcers that can aid in healing and improve outcomes. Some of these treatments include:
- Negative pressure wound therapy (NPWT): NPWT involves applying a vacuum system to the wound, which helps remove excess fluid and promotes blood flow, thereby accelerating wound healing. It can be particularly beneficial for large or complex foot ulcers.
- Hyperbaric oxygen therapy (HBOT): HBOT involves breathing pure oxygen in a pressurised chamber, which increases the oxygen level in the blood and tissues. This can enhance wound healing and fight off infection.
- Antibiotics and antimicrobial agents: In cases of infected foot ulcers, antibiotics or antimicrobial agents may be necessary to manage the infection and prevent its spread.
Recommended diabetic wound healing ointments and creams
Regarding diabetic wound healing, several over-the-counter (OTC) ointments and creams can help promote healing and prevent infection. While it’s essential to consult with a healthcare professional before using ointments, here are some commonly recommended options:
- Foot creams: OTC antibiotic ointments, such as Diafoot Sb Cream, can be applied to clean wounds to prevent infection. These creams typically contain ingredients that moisturise and protect the diabetic foot.
- Hydrogel ointments: These ointments, such as Medihoney Gel or Aquaphor Healing Ointment, can create a moist environment that helps heal wounds. They provide a soothing effect and promote a favourable environment for tissue regeneration.
- Petroleum jelly: Plain petroleum jelly, like Vaseline, can be a protective barrier on minor wounds to keep the area moist and prevent drying. It can also help reduce friction and promote healing.
- Aloe vera gel: Aloe vera gel, derived from the aloe plant, has soothing and healing properties. It can be applied topically to diabetic wounds to promote healing and relieve discomfort.
- Calendula ointment: Calendula ointment, made from the calendula flower, has anti-inflammatory and wound-healing properties. It can soothe and promote healing in minor cuts, burns, and wounds.
Proactive steps to prevent foot problems
- Improving the management of diabetes can help decrease the likelihood of nerve-related and blood pressure-related complications.
- Additionally, quitting smoking and regularly checking and properly trimming toenails can aid in preventing foot-related issues.
- It is important to promptly treat non-ulcerative conditions, such as tinea pedis or cracked heels, and wear appropriate footwear, such as well-fitting soft shoes or custom-made insoles.
- Engaging in exercise and physiotherapy can also be beneficial. Educating patients, their families, and healthcare providers is crucial to ensure proper care and prevent complications.
When to seek professional medical assistance
If you notice darkened skin around a foot ulcer where you can’t feel anything, it’s best to schedule a visit with your doctor as soon as possible. This can be a sign of an infected foot ulcer that requires immediate attention. Ignoring it could lead to the formation of abscesses, and the infection might even spread to other parts of your feet and legs.
Sometimes, you may need surgical intervention, an amputation, or synthetic skin substitutes to replace lost tissue. It’s crucial to take action early to avoid these complications.
Conclusion
Diabetic foot ulcers can be a significant concern for individuals with diabetes, but self-care practices can effectively prevent and treat them. It’s essential to prioritise proper foot hygiene, choose appropriate footwear, and manage blood sugar levels.
By implementing evidence-based recommendations and taking control of their foot health, individuals with diabetes can reduce the risk of difficulties and improve their quality of life. Remember, small changes in daily self-care practices can significantly improve overall foot health.
You can download our user-friendly Truemeds app to access medicines at low rates easily. Submit your prescription to our platform to receive branded and generic medications. Enjoy savings on purchases and the added convenience of free home delivery on relevant orders across India*.
Frequently asked questions
Several ointments can be used for diabetic foot ulcers, and the best one depends on the specific condition and individual. It is recommended to consult a doctor for appropriate ointment selection.
Betadine is generally not recommended for diabetic wounds as it can be cytotoxic to healthy tissues. It’s best to consult a healthcare professional for appropriate wound care products.
To prevent diabetic foot ulcers, you can take self-care measures such as daily foot inspections, proper foot hygiene, regular moisturisation, wearing comfortable and well-fitting footwear, and managing blood sugar levels.
If left untreated or poorly managed, diabetic foot ulcers can lead to severe complications that may require amputation. Early detection, proper wound care, and ongoing management are crucial in preventing such outcomes.
Diet plays a crucial role in preventing and treating diabetic foot ulcers. A well-balanced diet focusing on controlling blood sugar levels, maintaining a healthy weight, and providing essential nutrients can help promote wound healing and reduce the risk of complications.
Yes, diabetic foot ulcers can recur even after they have healed. It is important to continue practising preventive measures, ongoing foot care, and regular check-ups to minimise the risk of recurrence.
Various antiseptic solutions are available for diabetic foot care, and the choice depends on the wound condition and the healthcare professional’s recommendation. Commonly used solutions include chlorhexidine, povidone-iodine, and saline.
To clean a diabetic foot wound at home, wash your hands, gently cleanse the wound with mild soap and lukewarm water, and pat it dry. Apply antibiotic ointment if advised, cover with a sterile bandage, and change dressings regularly. Consult a healthcare provider for guidance, especially if there are signs of infection or uncertainty about wound care.
Disclaimer
The content provided within this article has been thoroughly verified for accuracy. However, we advise consulting a healthcare professional before utilising any medication or dietary supplements mentioned herein.
References
- American Diabetes Association Professional Practice Committee, American Diabetes Association Professional Practice Committee. 12. Retinopathy, neuropathy, and foot care: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2022 Jan;45(Supplement_1):S185-94. [Cited on 2023 June 22]. Available From: https://pubmed.ncbi.nlm.nih.gov/34964887/
- Foods EH, Weight MY. Type 2 diabetes-self-care. [Internet]. [Cited on 2023 June 22]. Available From: http://sbrmc.adam.com/content.aspx?productid=117&isarticlelink=false&pid=60&gid=000328
- National Institute of Diabetes and Digestive and Kidney Diseases website. Diabetes and foot problems. [Internet]. [Cited on 2023 June 22]. Available From: www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/foot-problems.
- Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Current diabetes reports. 2019 Oct;19:1-8. [Cited on 2023 June 22]. Available From: https://pubmed.ncbi.nlm.nih.gov/31456118/
- Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001;24(1):84–8. doi:10.2337/diacare.24.1.84. [Cited on 2023 June 22]. Available From: https://pubmed.ncbi.nlm.nih.gov/11194247/
- Everett E, Mathioudakis N. Update on the management of diabetic foot ulcers. Ann N Y Acad Sci. 2018;1411(1):153–65. doi:10.1111/nyas.13569. [Cited on 2023 June 22]. Available From: https://pubmed.ncbi.nlm.nih.gov/29377202/
Leave a Reply